healthcare professional
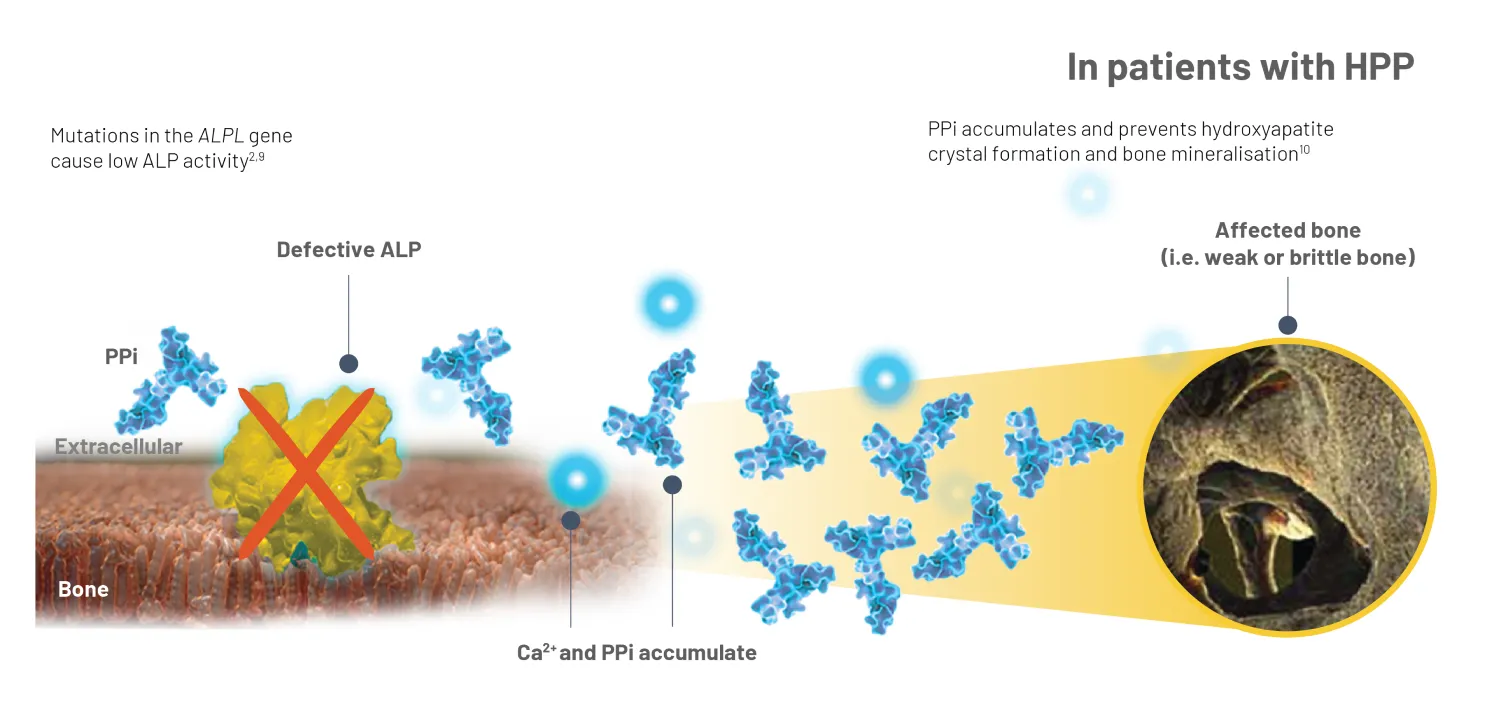
HPP is characterised by persistently low alkaline phosphatase (ALP) activity, and it is this key biochemical marker that is crucial to differentiating HPP from other conditions.6,7


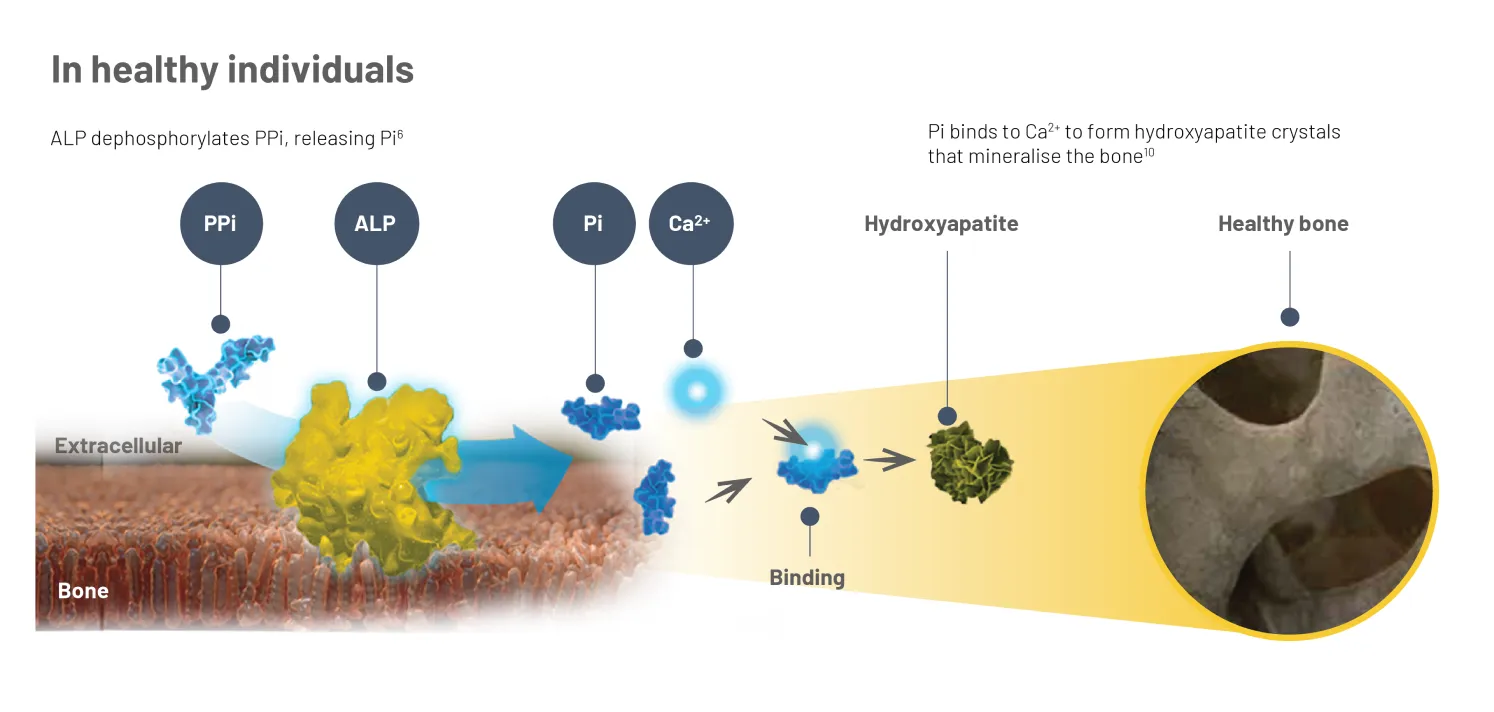
In healthy individuals, TNSALP hydrolyses inorganic pyrophosphate (PPi), a mineralisation inhibitor, to generate inorganic phosphate (Pi).4 Pi binds with calcium (Ca2+) to form hydroxyapatite crystals, the mineral matrix of bone.10
In HPP, deficient ALP leads to the accumulation of PPi and other substrates, leading to a range of skeletal defects and systemic complications.2,9
* Different isoforms of ALP exist; however, the majority is TNSALP,6,11 so throughout this webpage, it is referred to as ALP for simplicity.* Limitations: an ALP level of <40 U/L is not conclusive for a diagnosis of HPP. The patient should be evaluated for other symptoms of HPP, and differential diagnoses should be ruled out. Check with your lab for their appropriate age- and sex-adjusted ALP reference range.8
† The connection between ALP and PEA has not been fully established. PPi is also a substrate associated with HPP, however, tests for PPi are not commercially available.2Limitations: check with your lab for their appropriate age- and sex-adjusted ALP reference range.
ALP, alkaline phosphatase; Ca2+, calcium; HPP, hypophosphatasia; PTH, parathyroid hormone; PLP, pyridoxal 5’-phosphate; XLH, X-linked hypophosphataemia.