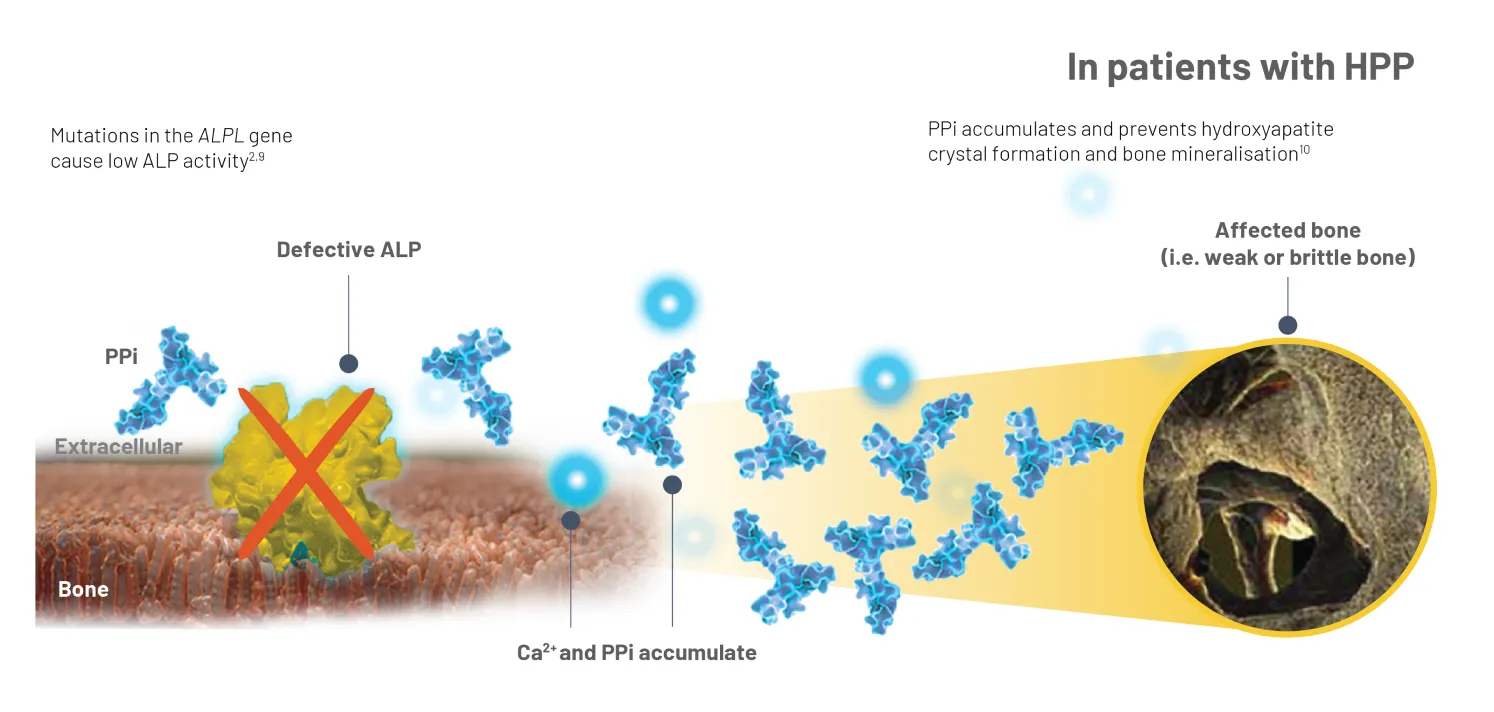
HPP is characterised by persistently low alkaline phosphatase (ALP) activity, and it is this key biochemical marker that is crucial to differentiating HPP from other conditions.6,7


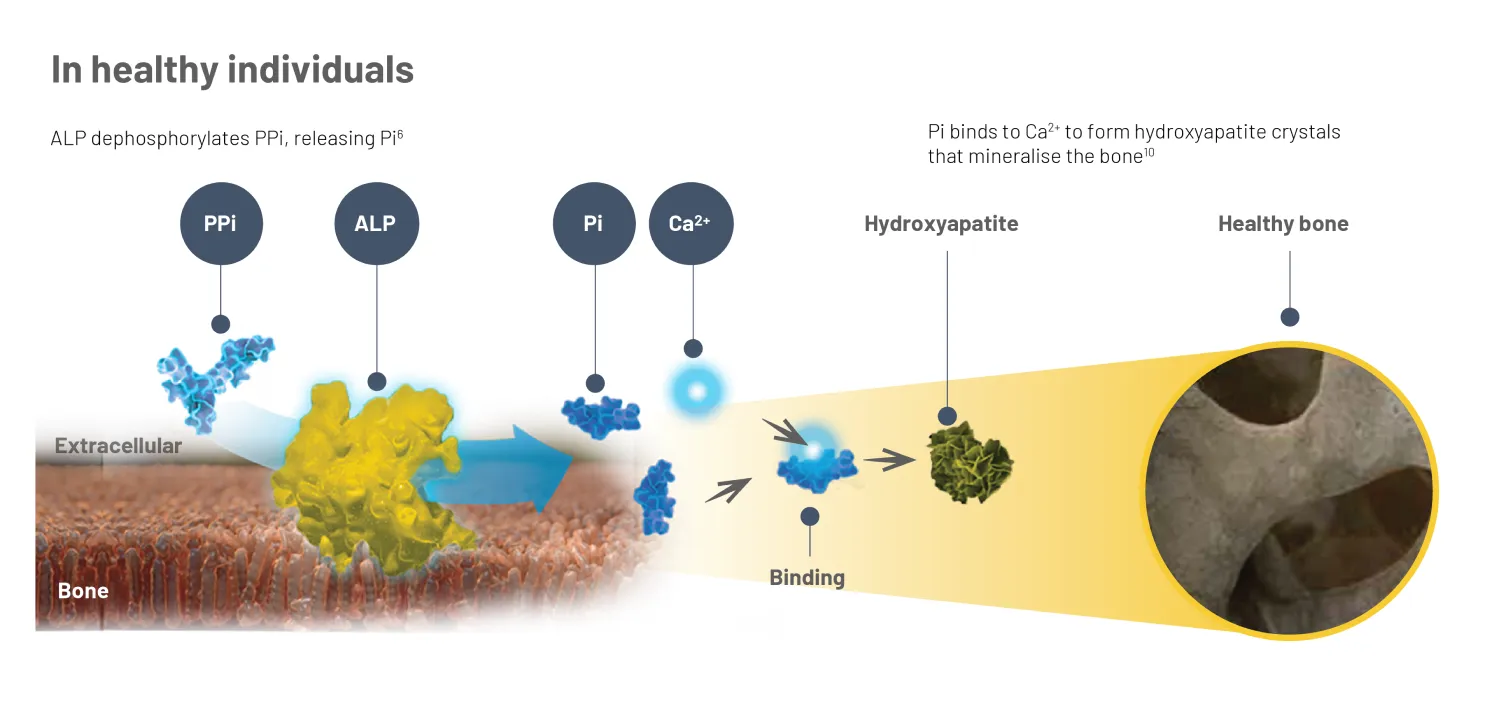
In healthy individuals, TNSALP hydrolyses inorganic pyrophosphate (PPi), a mineralisation inhibitor, to generate inorganic phosphate (Pi).4 Pi binds with calcium (Ca2+) to form hydroxyapatite crystals, the mineral matrix of bone.10
In HPP, deficient ALP leads to the accumulation of PPi and other substrates, leading to a range of skeletal defects and systemic complications.2,9
* Different isoforms of ALP exist; however, the majority is TNSALP,6,11 so throughout this webpage, it is referred to as ALP for simplicity.* Limitations: a low age and sex adjusted ALP level is not conclusive for a diagnosis of HPP. The patient should be evaluated for other symptoms of HPP, and differential diagnoses should be ruled out. Check with your lab for their appropriate age- and sex-adjusted ALP reference range.8
† The connection between ALP and PEA has not been fully established. PPi is also a substrate associated with HPP, however, tests for PPi are not commercially available.2Integral to the diagnostic evaluation are the considerations listed below. To support diagnosis of HPP in children or adults two major criteria or one major and two minor criteria are required, with the key diagnostic indicator being persistently low age- and sex-adjusted serum ALP activity levels. Confirming that the reduction in ALP is not due to another condition or drug is critical in following the diagnostic pathway2,8,9
Limitations: check with your lab for their appropriate age- and sex-adjusted ALP reference range.
ALP, alkaline phosphatase; Ca2+, calcium; HPP, hypophosphatasia; PTH, parathyroid hormone; PLP, pyridoxal 5’-phosphate; XLH, X-linked hypophosphataemia.