
Understanding NF1
Although NF1 is a genetic condition, only half of patients with the variant gene inherit it from a parent, while the other half develop it at random.1 An individual with the variant has a 50% chance of passing the variant on to their children.1
- Six or more ‘café-au-lait’ spots – discoloured, coffee-coloured patches on the skin
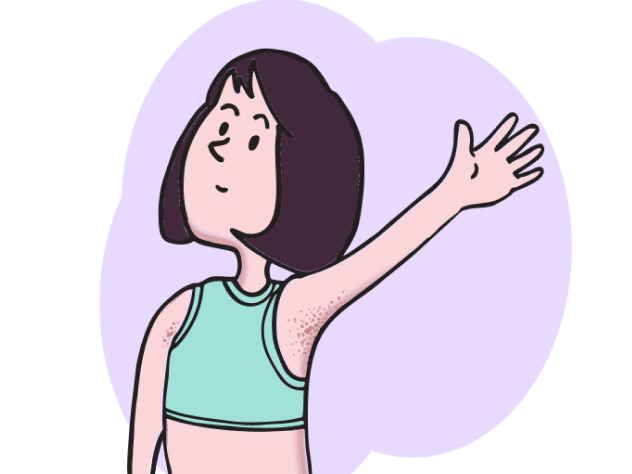
- Freckling in the armpit or around the groin area
- Two or more neurofibromas of any type or one plexiform neurofibroma (PN) – types of growths on nerves
- Optic pathway glioma – a slow-growing brain tumour around the optic nerve
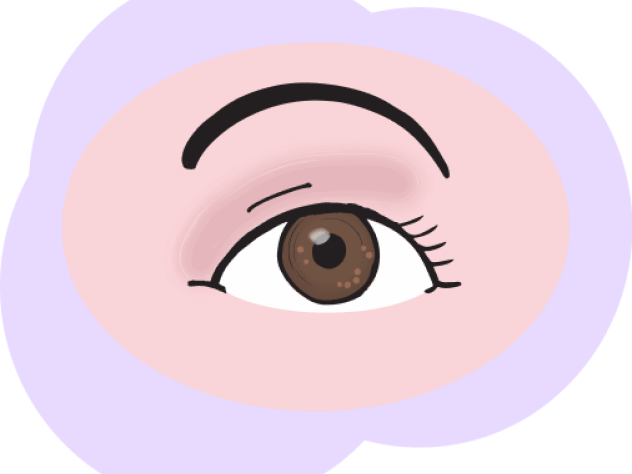
- Two or more dome-shaped masses on the surface of the iris (Lisch nodules), or two or more bright patches in the white part of the eye (choroidal abnormalities)2
- A distinctive bone lesion – an abnormal change to one or more bones
- A defective version of the NF1 gene that is responsible for the disease, which is present in 50% of apparently normal tissue, such as white blood cells
1. ‘Café-au-lait’ spots
Café-au-lait spots, discoloured, coffee-coloured patches on the skin, are present in 99% of people with NF1 and first appear from birth up to 12 years of age.4
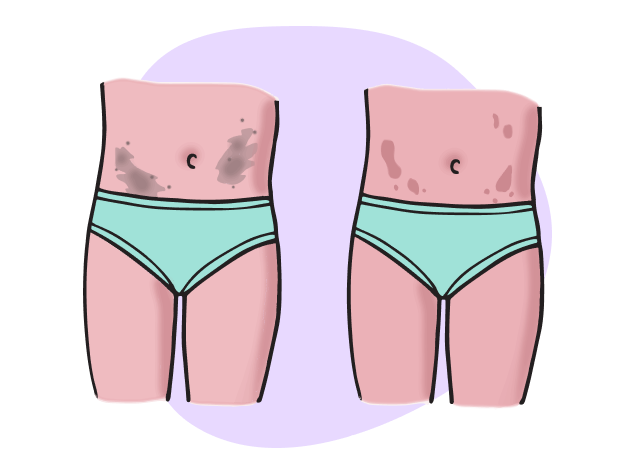
2. Freckling
Freckling in the armpits or around the groin is present in 85% of people with NF1 and may first appear from 3 years of age to adolescence.4
3. Neurofibromas
Neurofibromas are benign (non-cancerous) tumours that grow along the length of nerves.4 They can bulge out of the skin (cutaneous) or stay just under the surface (subcutaneous).4 Neurofibromas are present in 99% of people with NF1 and appear after 7 years of age, typically in late adolescence.4
PN are ‘interwoven’ tumours that can grow on nerves. PN can be seen or felt in up to 30% of people with NF1; however, they may be detected in up to 50% of people using whole-body imaging.4,5 They can first appear from birth up to 18 years of age.4

4. Optic pathway glioma
Optic pathway gliomas are tumours of the optic nerve that can be identified using magnetic resonance imaging (MRI) and are observed in 15% of people with NF1.4,5 They first appear from birth up to 7 years of age.4
5. Abnormalities of the eye
Signs of NF1 in the eye include Lisch nodules, which are lumps that grow in the iris (the coloured part of the eye) and are present in 90–95% of people with NF1.1,4 They tend to appear after 3 years of age.4
Choroidal abnormalities are bright, patchy spots and may also be seen by eye imaging examinations.2
6. Distinctive bone lesion
Distinctive bone lesions include defects to the skeleton, for example, scoliosis (curved spine) and sphenoid wing dysplasia.1,4
Sphenoid wing dysplasia is characterised by an undersized or absent sphenoid (a bone that forms part of the skull around the eyes) and is present in less than 1% of people with NF1.4,6 It is found at birth if present.4
Other distinctive lesions include curving (bowing) of the shin bone and long bone fractures that do not heal.3
7. NF1 gene variant
Genetic testing can be performed to identify a disease-causing NF1 gene variant.5 This variant must be present in 50% of apparently normal tissue (e.g. white blood cells) for it to be considered indicative of NF1.1
PN aren’t always easy to notice in children with NF1. Sometimes they’re located deep inside the body, meaning they can’t be seen or felt.2 Sometimes they may be recognised by skin discolouration or a bump under the skin.2
PN can grow quickly in size and may cause other symptoms, including:4,7,8
- Pain
- Muscle weakness
- Visual impairment from PN around the eye
- Loss of bladder control
- Bowel issues, including severe constipation
- Airway issues, including the need for mechanical support
- Physical deformity
